The average person takes about 21,000 breaths a day. This makes it one of the 3 biggest aspects of our patients life that we can have a profound effect on (other 2: posture & walking).
This post will discuss the holistic effects of breathing, anatomy, and the important cascade of events for proper breathing and inner core stabilization.
Why Work On Breathing?
Because everyone is doing it. Power lifters have been controlling their intra-abdominal pressure to lift massive weights for years. Yoga and eastern medicine have been using breathing for over 2,000 years (PT isn’t even a century old) . Gray Cook and the SFMA require a full breath at the end-range of every movement test to achieve a FN. The neuro-orthopedic approach leans on breathing and even mentions that a deep breath glides the median nerve 1 inch. There is an increasing amount of approaches that are including breathing (PRI, SFMA, DNS). Many of the leading experts in the field are incorporating breathing. And there is more and more research coming out discussing the benefits of breathing. So if you’re not doing it, or at least aware of it, then you are probably that guy.
Holistic Breathing
Breathing has a huge influence on the entire body. Breathing influences sympatho-vagal balance. Dyfunctional breathing can induce hypocapnia (effect of hyperventilation). Hypocapnia causes increased neural activity and synaptic transmission. You know those patients that feel that every muscle is tight and you can never decrease their muscle tone for more than 24 hours? Maybe it’s because of their breathing. Breathing can actually produce an amplification of the parasympathetic nervous system. This can have a tremendous effect on muscle tone (a nervous system issue).
Breathing also has a significant role in the circulatory system, pH regulation, and metabolism. It has been tied to many psychological disorders and can have a major effect on self-regulation of stress and emotion. Breathing even has an important role in some religions and spiritual practices.
Breathing has a therapeutic, homeostatic, regulatory, psychophysiological, and spiritual function. If your patients are alive, then breathing should be considered as an aspect of their care.
Breathing Anatomy
A global understanding of breathing anatomy can be expanded from knowledge of the deep front line. This line from Anatomy Trains goes into the fascial attachments of the diaphragm in great detail. Or simply stated, “the 12th rib is where walking meets breathing“-Tom Myers.
Diaphragm
The diaphragm has a dual function: respiration and stability. It should be able to perform this dual function at all times. A common injury is caused by a failure of this mechanism. The overweight, sedentary, desk-jockey wakes up to shovel snow out of his driveway. After 5 minutes he’s exhausted and his diaphragm has to devote all of its power for respiration. Now his diaphragm has lost it’s stability function. Now he can’t control and use his intra-abdominal pressure (IAP). And now he just hurt his back.
Want another reason why we should know about the diaphragm’s stability role? It’s the most proximal muscle…to everything. There’s nothing more proximal than the diaphragm. It helps to organize and stabilize the upper and lower quarter. Sue Falsone agrees that the diaphragm is the most proximal. Regarding this concept she has said that she always starts rehab “from the belly button out.”
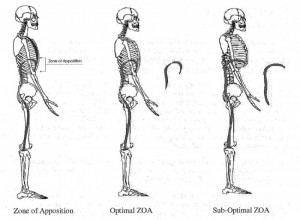
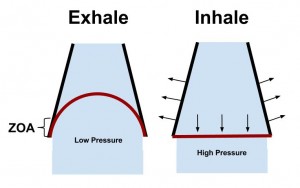
Zone of Apposition
The Postural Restoration Institue defines the ZOA as the “cylindrical aspect of the diaphragm that apposes the inner aspect of the lower mediastinal (chest) wall.” This is one of the most important aspects of breathing. The ZOA is responsible for:
- Efficient length-tension relationships of the diaphragm
- Maintains vertical alignment of diaphragm muscle fibers
- Allows postero-lateral (bucket-handle) movement of the lower rib cage
Overall the ZOA is paramount for proper diaphragm function. Some have found it to be as much as 30% of the inner surface of the ribcage. A decreased ZOA will result in inefficient diaphragm contraction, lung hyperinflation, increased accessory muscle use, lack of postero-lateral movement of the rib cage, and an increased anterior rib flare.
Abdominals & Pelvic Floor
The abdominals and pelvic floor play a huge role in inspiration (eccentrically) and expiration (concentrically). During inspiration they contract eccentrically to increase the intra-abdominal pressure (i.e. stability) and ensure that the ZOA is maintained long enough to produce postero-lateral expansion of the lower ribcage. During expiration they concentrically contract to help push the diaphragm cephallically, thus restoring optimal ZOA.
Thoracic Cavity
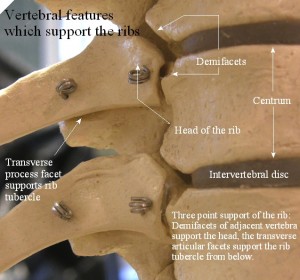
The thoracic cavity is where the actual breath occurs. It’s where the air molecules and gas exchange occurs. The thoracic cavity must have the appropriate amount of mobility to accommodate this pressure change and flow of molecules. During inspiration the ribs must be able to ER and the spine must be able to extend. During expiration the ribs must be able to IR and the spine must be able to flex.
Breathing plays a major role in the hydration of the thoracic discs. If you look at the anatomy of the ribs attachment to the thoracic spine it almost looks like a lever. This lever actually pry’s open the thoracic spine and elongates it, thus bringing hydration and nutrition to the discs.
Breathing Mechanics (Core from the Inside Out)
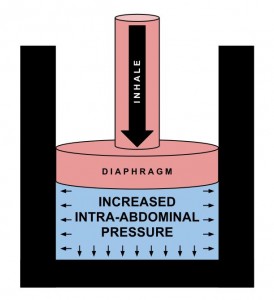
There is a cascade of events that leads to controlled intra-abdominal pressure through the activation of the diaphragm and core musculature. By using the breath with the core you are achieving natural muscle activation and increased intra-abdominal pressure. This pressurized stability is much more efficient than muscle activation alone (abdominal hallowing/isolated TVA activation).
The best way to have a proper breathing pattern is to get it right from the inhale. A proper inhale will put you in the correct position for a proper exhale. Clinically there are many things that can go wrong with inspiration, whereas the only thing that often goes wrong with expiration is decreased expired air (hyperventilation/decreased ZOA).
The inhale is the initiation of core stability.
Inspiratory Cascade of Events
1) Diaphragm Concentrically Contracts
2) Beginning of Increased IAP
3) Abdominals and PF Eccentrically Contract
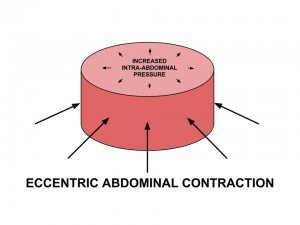
Increased IAP is optimized with an eccentric contraction of the abdominals & PF. This maintains ZOA and causes 3-dimensional expansion of the lower ribcage.
4) Controlled Increase in IAP & Inner Core Stability
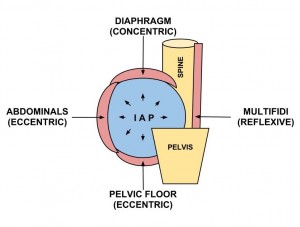
The effect of a proper inhale results in controlled IAP via trunk musculature. The increased IAP anterior to the spine causes a reflexive activation of the posterior spinal stabilizers.
Bottom Line
Understanding breathing anatomy and mechanics will allow you to easily assess and intervene respiration. The effects of proper breathing are: adequate respiration, proper biochemical balance, decreased/prevention of psychological distress, and most important for physical therapist – natural activation of the inner core stability. Part II will deal with ideal & dysfunctional breathing patterns, assessment, and some simple interventions.
Dig Deeper
Hans Lingren – Core Stability Inside Out
SportsRehabExpert – Ron Hruska Interview
Mike Robertson – Video Coaching
References
Tom Myers & Leslie Kaminoff. The Breath in the Pelvis – Seminar (NYC 2012).
Courtney R,Reece J (2009). Comparison of the Manual Assessment of Respiratory Motion (MARM) and the Hi Lo breathing assessment determining a simulated breathing pattern. International Journal of Osteopathic Medicine.
Courtney R (2009). The functions of breathing and its dysfunctions and their relationship to breathing therapy. International Journal of Osteopathic Medicine
Courtney R (2011). Dysfunctional Breathing – It’s paramaters, measurement and relevance. Thesis RMIT University. (a must read – click here)
Kaminoff L. (2006). “What yoga therapists should know about the anatomy of breathing.” International Journal of Yoga Therapy.
McLaughlin L. (2009). “Breathing evaluation and retraining in manual therapy.” Journal of Bodywork and Movement Therapies.
McGill S , Sharratt M ,Sequin J P. (1995). “Loads on spinal tissues during simultaneous lifting and ventilatory challenge.” Ergononomics.
Janssens L , Brumagne S, Polspoel K, Toosters T, McConnell A. (2010). “The effect of inspiratory muscles fatigue on postural control in people with and without recurrent low back pain.” Spine.
Hodges P , Heijnen I, Gandevia S C. (2001). “Postural activity of the diaphragm is reduced in humans when respiratory demand increases.” Journal of Physiology.
Hodges P , Butler J ,Mackenzie D K, Gandevia S C. (1997). “Contraction of the human diaphragm during rapid postural adjustments.” Journal of Physiology 505(Pt. 2
Wang S., McGill S (2008). Links Between the Mechanics of Ventilation and Spine Stability. Journal of Applied Biomechanics.
McGill S, Sharratt M & Seguin J (1995). Loads on the spinal tissues during simultaneous lifting and ventilatory challenge. Ergonomics.
Robey J, Boyle K (2009). Bilateral Functional Thoracic Outlet Syndrome in a College Football Player. N Am J Sports Phys Ther.
Boyle K, Olinick J, & Lewis C (2010). The value of blowing up a balloon. N Am J Sports Phys Ther.
Kolar P, Sulc J, Kyncl M, et al. (2010) Stabilizing function of the diaphragm: dynamic MRI and synchronized spirometric assessment. J Appl Physiol.
Kolar P, Sulc J, Kyncl M, et al. (2012). Postural Function of the Diaphragm in Persons With and Without Chronic Low Back Pain. JOSPT.
Hagins M, Lamberg EM (2011). Individuals with low back pain breathe differently than healthy in- dividuals during a lifting task. JOSPT.
Clifton-Stmith T, Rowley J (2011). Breathing pattern disorders and physiotherapy: inspiration for our profession. Physical Therapy Review.
Hruska R (2005). ZOA Position & Mechanical Function. Postural Restoration Institue.
Cook, Gray. Movement: Functional Movement Systems : Screening, Assessment, and Corrective Strategies. Aptos, CA: On Target Publications, 2010.
—
The main reason I do this blog is to share knowledge and to help people become better clinicians/coaches. I want our profession to grow and for our patients to have better outcomes. Regardless of your specific title (PT, Chiro, Trainer, Coach, etc.), we all have the same goal of trying to empower people to fix their problems through movement. I hope the content of this website helps you in doing so.
If you enjoyed it and found it helpful, please share it with your peers. And if you are feeling generous, please make a donation to help me run this website. Any amount you can afford is greatly appreciated.